Laser Prostatectomy
You have an enlarged prostate gland. This is also called benign prostatic hyperplasia (BPH). BPH is not cancer, but it can cause problems with urination. To ease your symptoms, your healthcare provider may advise laser prostatectomy . This procedure uses a laser (concentrated light energy). The laser removes excess prostate tissue from around the urethra. The urethra is the tube that carries urine from the bladder out of the body. The surgery lets urine flow more freely through the urethra by removing the pressure of excess tissue.
Types of prostate laser surgery
The type of laser surgery your healthcare provider will do may depend on your health, the size of your prostate, and the type of tools available. The different types of prostate laser surgery are:
-
Photoselective vaporization of the prostate (PVP). The laser is used to melt away (vaporize) the extra prostate tissue.
-
Holmium laser ablation of the prostate. This type of surgery is similar to PVP. But it uses a different kind of laser.
-
Holmium laser enucleation of the prostate (HoLEP). In this procedure, the laser cuts and removes extra tissue. A tool cuts the tissue into small pieces. This makes them easier to remove.
-
Thulium laser enucleation of the prostate . This type of surgery is similar to HoLEP, but it uses a different kind of laser.
Possible risks and side effects of laser prostatectomy
All procedures have risks. Some possible risks of this procedure include:
-
Bleeding
-
Infection
-
Urgency and burning when you pee
-
Blood clots
-
Scarring or narrowing of the urethra. This can cause trouble peeing.
-
Only some relief of symptoms
-
Erectile dysfunction (rare)
-
Loss of bladder control (very rare)
-
Loss of ejaculation
Getting ready for the procedure
Your healthcare team will give you detailed instructions on how to get ready for the procedure. Be sure to follow them.
-
You will be asked to read and sign a form consenting to the surgery. Be sure to read the entire document. Have all of your questions answered before signing it.
-
Tell your healthcare team about all medicines you take. This includes prescription and over-the-counter medicines, vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, or daily aspirin. You may need to stop taking some or all of them before surgery.
-
Follow any directions you're given for not eating or drinking before your procedure.
-
When you arrive for the procedure, you'll have an IV (intravenous) line placed. This gives you fluids and medicines during the procedure.
-
You'll be given medicine to keep you from feeling pain (anesthesia) before the procedure. You may have one or more of the following:
-
Local anesthesia. Your bladder and urethra are numbed.
-
Regional anesthesia. Your body below the waist is numbed. You may also be given medicine to make you drowsy.
-
General anesthesia. You are sleeping comfortably during the entire procedure.
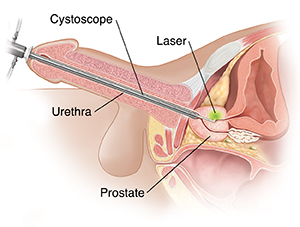
During the procedure
Your healthcare provider can help explain the details of your surgery. These details depend on the type of laser surgery that will be done. In general, you can expect the following:
-
The procedure itself often takes less than 1 hour.
-
A thin, tube-like telescope (cystoscope) is put through the opening in your penis and into your urethra. This tool lets your provider see your urethra and your prostate. They are seen either through the cystoscope or on a screen.
-
The laser is put through the cystoscope. The laser is then used to destroy the extra prostate tissue.
-
You may have a tube (urinary catheter) to help your bladder drain urine for a short time after the procedure. It’s removed when it’s no longer needed.
After the procedure
You may go home the same day after your surgery. Or you may stay a night in the hospital for observation. An adult friend or family member should drive you home. To get the best results from the procedure, follow your healthcare provider's instructions. Keep your follow-up appointments.
Your prostate will likely be sore at first. This will get better as you heal. Here are some things you can expect:
-
You may be sent home with a catheter to drain urine from your bladder. If so, you may wear a leg bag until it's no longer needed. The catheter will allow the area to heal. It will help prevent painful urination.
-
Your provider may also prescribe antibiotics to prevent infection and pain medicine to ease any discomfort.
-
In about 1 week, you’ll visit your healthcare provider to have your catheter removed. If swelling still makes it hard to pee, the catheter may be left in longer. After the catheter is removed, you may need to pee more often. This is normal and should get better with time.
-
For the first few weeks after your procedure, you may notice that your urine is cloudy. Or you may have blood or blood clots in your urine. This is normal while your body rids itself of the treated tissue. These symptoms may start to get better during the first few weeks. But it may take a few months before they go away. Your healthcare provider can tell you when you can have sex again and when you can go back to work.
-
You also may be told to not lift anything over 10 pounds. And to not bend over or strain to lift things from the ground.
-
Drink plenty of fluids to help flush out your bladder.
Getting back to sex
You may be glad to know that BPH and its treatments rarely cause problems with sex. You may find that you have retrograde ejaculation. This happens when semen goes into the bladder instead of the urethra during ejaculation. Retrograde ejaculation is common after procedures for BPH. But even if this does occur, orgasm shouldn’t feel any different than it did before the procedure. And it shouldn't cause any health problems or affect your sexual function. If you notice any problems with sex, talk with your healthcare provider. Help may be available.
When to call the healthcare provider
Contact your healthcare provider right away if:
-
You have a fever of 100.4°F (38°C) or higher, or as directed by your provider
-
You have excessive bleeding
-
You have pain not relieved by medicines
-
You notice that no urine is draining from the catheter, or the catheter falls out
-
You have a frequent or very strong urge to pee
-
You’re not able to pee, or notice a decrease in urine flow
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
8/1/2023
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.