A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
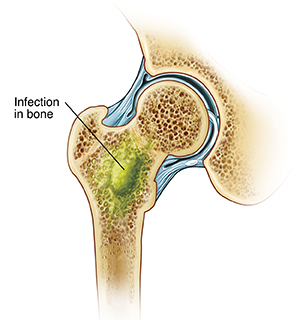
When Your Child Has Osteomyelitis
Your child has been diagnosed with osteomyelitis. This is an infection of a bone by a germ (bacteria or fungus). In children, infection in the long bones of the arms and legs is most common. Your child may be referred to an orthopedist (specialist in bone and joint problems) or an infectious disease specialist (specialist in infections) for evaluation and treatment.
What causes osteomyelitis?
Germs such as bacteria and fungi can cause osteomyelitis. The most common type of bacteria that causes osteomyelitis is called Staphylococcus aureus or staph. The bacteria and fungi can enter the body through:
-
Infected wounds or joints
-
Infections that spread from another part of the body
-
Broken bones that break through the skin
-
Foreign object that breaks the skin
Those at higher risk for bone infection include children:
But any child can get this infection. In some cases, the cause of the infection is never known.
What are the symptoms of osteomyelitis?
If your child has any of these symptoms, get medical help right away.
-
Fever of 100.4°F ( 38°C) or higher, or as advised by your child's provider
-
Chills
-
Pain in the bone
-
Swelling of the arms or legs
-
Redness or warmth of the skin on the arms or legs
-
Pus draining from the skin
-
Not letting the arms or legs be touched
-
Not using the arms or legs (limb unable to hold weight)
-
Babies could be irritable or lethargic, refuse to eat, or vomit.
An infection often happens from a recent injury. Symptoms of the infection are masked by the symptoms of the injury. Because of this, it might take longer to notice the infection. It's important to bring your child to their healthcare provider if symptoms don't get better quickly.
How is osteomyelitis diagnosed?
If the healthcare provider thinks your child may have osteomyelitis, these tests may be done:
-
X-ray of the area to look for infection
-
Blood tests to confirm infection and find the germ causing the infection
-
Imaging tests such as a bone scan, CT scan, MRI, or ultrasound
-
Biopsy (procedure to take a sample of bone) to find the germ causing the infection
How is osteomyelitis treated?
At first, treatment often takes place in the hospital. The treatment may include:
-
Antibiotic or antifungal medicines, given through an IV (intravenous) line or by mouth (oral)
-
Pain medicine
-
Surgery to clean out infected area in and around the bone
Your child may be given antibiotics for 4 to 6 weeks. This can be done using a PICC line (peripherally introduced central catheter) at home. In other cases, your child may be able to have oral antibiotics. This will depend on how they've responded and the specific germ causing the infection.
Long-term concerns
Most children recover completely. Although rare, complications can occur. They include:
-
Blood clots
-
Growth problems
-
Abnormally shaped bones
-
Broken bones (fractures)
-
Joint stiffness
-
Death of bone tissue
Online Medical Reviewer:
Raymond Turley Jr PA-C
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Online Medical Reviewer:
Thomas N Joseph MD
Date Last Reviewed:
6/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.