When Your Child Has Chickenpox
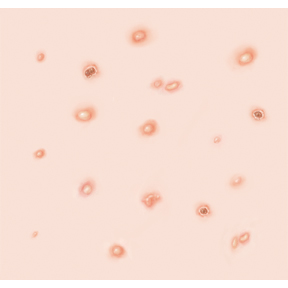 |
| Chickenpox causes an itchy rash that appears as bumps and blisters, which can spread all over the body. |
Chickenpox is an illness that can easily spread from person to person (contagious). It causes an itchy skin rash that appears as bumps and blisters. The rash can spread all over the body. Though chickenpox can cause some discomfort, most children recover with no lasting effects. In the past, chickenpox was very common and could not be prevented. A vaccine is now recommended to protect your child from getting it. It's given in 2 doses: at ages 12 to 15 months and ages 4 to 6 years. If your child has not received the vaccine, ask your child’s healthcare provider for more information.
What causes chickenpox?
Chickenpox is caused by the varicella-zoster virus.
What are the symptoms of chickenpox?
Symptoms can appear 10 to 21 days after exposure. The following symptoms usually occur before the rash:
-
Fever
-
Tiredness
-
Muscle aches
-
Loss of appetite
The rash usually occurs on the face, chest, and back. It starts as small, red bumps that turn into blisters. These blisters then crust and scab over.
How is chickenpox spread?
Chickenpox can be spread in the following ways:
-
Through direct contact with the rash on an infected person
-
Through the air when an infected person coughs or sneezes
-
Through direct contact with the rash on a person who has shingles. (Shingles is an illness caused by the chickenpox virus. It affects adults who have had chickenpox or picked up the virus in the past.)
How is chickenpox diagnosed?
-
If you suspect that your child has chickenpox, let your healthcare provider know before your child’s appointment. This is to reduce the risk of spreading it to other children at the provider's office.
-
Chickenpox is usually diagnosed by how the rash looks. Your healthcare provider will examine your child and ask about your child’s symptoms and health history. A blood test may be requested to confirm diagnosis.
How is chickenpox treated?
-
Chickenpox generally lasts about 7 to 10 days.
-
Your child is contagious for 1 to 2 days before the rash starts. They should not attend school or daycare until the blisters caused by the rash have crusted over.
-
In some cases, especially if your child has a weak immune system, your child's healthcare provider may advise an antiviral prescription medicine. This medicine works best if taken within 24 hours after the rash starts.
-
You can do the following at home to relieve your child’s symptoms:
-
Give your child over-the-counter (OTC) medicines, such as ibuprofen or acetaminophen, to treat pain and fever. Don't give aspirin to a child with a fever. This can put your child at risk of a serious illness called Reye syndrome. Don't give ibuprofen to an infant who is 6 months of age or younger.
-
Give your child OTC antihistamine medicine to ease itching.
-
Apply calamine lotion to the rash to relieve itching. Before and after each application, wash your hands with warm water and soap.
-
Give your child an oatmeal bath. This can soothe the skin and relieve itching. Some oatmeal mixes can leave an oily film in the tub. To prevent falls, make sure to clean the tub well before the next person uses it.
When to call your child's healthcare provider
Call your child's healthcare provider right away if your otherwise healthy child has any of the following:
-
Symptoms that don't improve within 7 days of starting treatment
-
A fever (see Fever and children, below)
-
Rash spreads near the eyes
-
Rash shows signs of infection (pus or drainage)
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° (38°C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older