A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Paracentesis
Your healthcare provider recommends that you have paracentesis. This is a procedure to remove extra fluid from your belly (abdomen). A needle is used to drain the fluid. A small sample of fluid may be taken and tested for problems. If the fluid buildup is causing discomfort or pain, all of the fluid may be drained. To do this, a tube is attached to the needle. The fluid is drained into a container that sits outside of the body. If symptoms are severe, paracentesis may be done as an emergency procedure. Otherwise, it will be scheduled ahead of time. Read on to learn more about paracentesis and how it works.
Understanding ascites
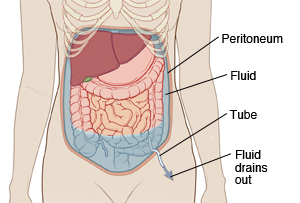
Many of the body’s organs, including the liver and intestines, are inside the belly. The organs are covered in a thin membrane called the peritoneum . The peritoneum has 2 layers. It makes a fluid that allows the layers to glide smoothly past each other. If this fluid builds up in the belly, the condition is called ascites . Ascites causes pain and discomfort. It can also make it hard to breathe. Fluid can build up for a number of reasons. These include chronic liver disease (cirrhosis), heart or kidney failure, and cancer. Your healthcare provider can tell you more about the cause of your ascites.
How paracentesis works
The goal of paracentesis may be to help diagnose the cause of the excess fluid. Or the goal may be to drain excess fluid from the abdomen. In some cases, fluid returns. And the procedure needs to be repeated.
Before the procedure
-
Before the procedure, you will be asked to sign an informed consent. This form states that you understand the risks and benefits of the paracentesis. It also states any questions you have were answered. Be certain to ask all of your questions before you sign.
-
Tell your healthcare provider about any medicines you are taking. This includes all prescription medicines, over-the-counter medicines, street drugs, herbs, vitamins, and other supplements.
-
Tell your provider about any allergies you have.
-
Before the procedure begins, you’ll be asked to empty your bladder. This helps prevent injury to the bladder during the procedure. If needed, a thin tube (Foley catheter) may be placed into your bladder to drain urine during the procedure. This tube is removed after the procedure.
-
An IV (intravenous) line may be put into a vein in your arm or hand. This line supplies fluids and medicines.
During the procedure
-
You are awake during the procedure.
-
An imaging method called ultrasound may be used to guide the procedure. It shows live images of the inside of your belly on a video screen. This helps the provider find the site of the excess fluid inside your belly and decide where to insert the needle.
-
A numbing medicine (local anesthesia) is injected into your belly where the needle will be inserted.
-
Once the skin is numb, the healthcare provider carefully inserts the needle into the belly. This causes the needle to fill with fluid.
-
The needle may be removed with only a small sample of fluid. This sample is sent to a lab for testing. Getting a sample takes about 10 to 15 minutes.
-
Or, a tube may be attached to the needle so that more of the excess fluid can be drained. The tube may be taped or stitched into place. This keeps it from pulling the needle out of your belly.
-
How long it takes to drain all of the fluid varies for each person. In most cases, it takes about 30 minutes. Your provider will let you know if the procedure is expected to take longer than usual.
-
Once all of the fluid is drained, the needle and tube are removed.
-
Pressure is put on the puncture site to stop any fluid leakage or bleeding.
-
A small bandage is placed over the puncture site. Albumin may be given during or after the procedure to prevent low blood pressure or kidney problems.
After the procedure
You may be taken to a recovery room to rest after the procedure. If you are in pain, you will be given medicine as needed. You will likely be sent home 1 to 2 hours after the procedure is done. When you leave the hospital, have an adult family member or friend drive you home. If you are staying in the hospital, you will return to your hospital room. If your fluid is infected, you will be sent home on antibiotics. In some cases, the paracentesis may need to be repeated if the fluid returns. You may need to take medicines that increase urination (diuretics) to decrease fluid buildup. Because the tests on the fluid may take some time, be sure to follow up with your provider about your results.
Risks and possible complications of paracentesis
This procedure is considered safe. But like all procedures, it carries some risks. These include the following:
-
Bleeding
-
Infection
-
Injury to structures in the belly
-
Fast drop in blood pressure
-
Kidney problems after the procedure
When to get medical care
Call your healthcare provider if you notice any of the following after the procedure:
-
A fever of 100.4° F ( 38.0°C) or higher, or as directed by your provider
-
Chills
-
Trouble breathing
-
Pain that does not go away even after taking pain medicine
-
Belly pain not caused by having the skin punctured
-
Bleeding from the puncture site
-
More than a small amount of fluid leakage from the puncture site
-
Swollen belly
-
Signs of infection at the puncture site. These include increased pain, redness, or swelling, as well as warmth or bad-smelling drainage.
-
Blood in your urine
-
Dizziness, lightheadedness, or fainting
Online Medical Reviewer:
Jen Lehrer MD
Online Medical Reviewer:
L Renee Watson MSN RN
Online Medical Reviewer:
Marianne Fraser MSN RN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.