A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of medical procedures beginning with that letter.
Click 'Back to Intro' to return to the beginning of this section.
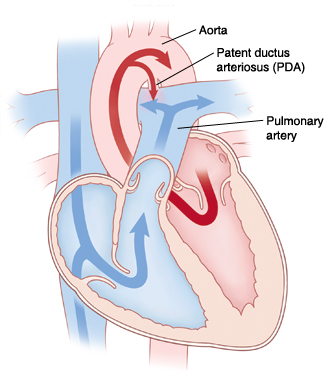
Patent Ductus Arteriosus (PDA) in Premature Infants
Your infant has been diagnosed with a patent ductus arteriosus (PDA). The ductus arteriosus is a normal structure in a fetus’s heart before birth. It’s a blood vessel that connects 2 arteries: the pulmonary artery and the aorta. The pulmonary artery carries blood from the heart to the lungs. The aorta carries blood from the heart to the body. Before birth, the ductus arteriosus allows blood from the right ventricle to bypass the lungs because the fetus gets oxygen from the mother. The ductus arteriosus normally closes shortly after birth once the baby breathes on its own. It’s called a PDA when it stays open (patent). A PDA can lead to worsening heart function over time. But it can be easily treated. In the United States, this is a fairly common congenital (present at birth) heart defect. A PDA is more common in premature infants, but it can also be seen in full-term infants. It may be associated with other congenital heart defects. It is more common in girls.
 |
| If the ductus does not close soon after birth, too much blood may go to the baby’s lungs. |
When is the PDA a problem?
A PDA that remains open beyond a few days after birth can strain the heart and increase the blood pressure in the lungs. This can cause fluid to build up in the lungs (pulmonary congestion) and may make it hard for the baby to breathe. The heart also has to work harder.
How is PDA diagnosed?
The problem can be detected with an echocardiogram. This is an ultrasound imaging test of the baby’s heart. In mild cases, there may be no symptoms. Or symptoms can include:
-
A heart murmur
-
Poor growth or weight gain
-
Sweating during feeding
-
Rapid breathing or trouble breathing
-
Decreased exercise tolerance in the older child
How is PDA treated?
The ductus may close on its own without treatment. If it doesn’t, treatments include:
-
Medicine. Certain medicines such as nonsteroidal anti-inflammatory drugs (NSAIDs) can narrow the artery. This shrinks the duct and allows it to close. The medicine is given by an IV (intravenous) line or by mouth over a period of a few days. During this time, the baby is watched closely.
-
Catheter-based procedure. This is usually done on older or larger babies. This may be done on small- to moderate-sized PDAs if the treatment with medicine did not work. Children must be large enough to qualify for the procedure. A long, thin tube (catheter) is inserted into a larger artery in the leg. A small metal coil or device is pushed through the catheter to the PDA. It is placed like a plug to block blood flow between the vessels. The coil or device is released and stays there long-term (permanently).
-
Surgery. This may be done if your baby can’t tolerate the medicine, or if treatment with medicine has not worked. Typically, it is done on children who are too small for a catheter-based procedure, or if a catheter-based procedure was not successful. The surgeon may advise surgery if other related congenital heart defects need surgery. The surgeon makes a cut (incision) between the ribs on the left side of the chest and clamps or ties off the opening in the blood vessel. The surgery doesn’t involve the heart muscle. This surgery has a high success rate and a low risk for complications.
What are the long-term effects?
Once the ductus is closed, there are rarely long-term complications. After closure using catheter-based procedures, preventive antibiotics may be given to prevent infection when your child has other procedures like dental work. Ask your cardiologist about what activities are safe for your baby.
Online Medical Reviewer:
Amy Finke RN BSN
Online Medical Reviewer:
Scott Aydin MD
Online Medical Reviewer:
Stacey Wojcik MBA BSN RN
Date Last Reviewed:
3/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.