Lumpectomy
Lumpectomy is surgery to remove a mass or lump in the breast along with a small amount of healthy tissue surrounding it. The mass may or may not be cancer. It's also called breast-conserving surgery because much of your breast remains unchanged.
There will be one cut (incision) on your breast for the lumpectomy procedure. You may have a second incision in your arm pit if lymph nodes will be removed and checked for cancer.
The mass along with surrounding breast tissue that's removed will be sent to a lab for testing. If cancer is found, you and your healthcare provider will meet to discuss a treatment plan that is right for you. If cancer is found, you may need radiation treatment after your breast heals. This is done to help keep the cancer from coming back in the same breast. You may also need additional treatments for your cancer, such as chemotherapy or hormone therapy.
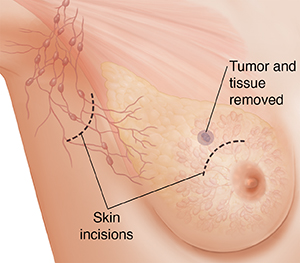 |
| You will have an incision near the tumor on the breast for the lumpectomy. You may also have a second incision under the arm, near the lymph nodes, for sentinel node biopsy or lymph node removal. |
Before surgery
An exam and some routine tests will be done about a week before the surgery. These help your surgeon know that you're well enough to have surgery. Before surgery:
-
Discuss risks of the surgery with your healthcare provider.
-
Sign any consent forms.
-
Tell your healthcare provider about any prescription or over-the-counter medicines, herbs, CBD, or supplements that you're taking. Tell your provider if you use marijuana or other substances.
-
Follow any directions you're given for not eating or drinking before your surgery.
-
Arrange for a trusted adult to drive you home after surgery.
-
Bring a soft shirt that buttons in front to wear home.
-
Talk with the anesthesia care provider. They'll explain how you'll be kept from feeling pain during surgery.
During surgery
Your surgeon will make an incision near the tumor. The tumor and an edge or margin of normal tissue will be removed. A second incision may also be made under the arm to remove some of the nearby axillary lymph nodes. These are checked to see if the cancer has spread to them.
When the surgery is finished, the incisions will be closed using stitches. A gauze dressing will cover the incisions.
Right after surgery
You'll wake up in a recovery room. You will have an IV (intravenous) line for fluids and medicines. Pain medicines will be given to you as needed. A nurse will check your temperature, pulse, and blood pressure. You'll most likely go home the same day.
You'll be given instructions on how to care for the incisions, what kind of pain medicines you should use, how to take care of yourself as you recover, and any changes in your activities. Make sure you understand all the instructions and know when you need to next see your healthcare provider.
Ask when you can expect the results of the surgery and when to make a follow-up appointment with your surgeon.
Risks of lumpectomy
All surgery has risks. Be sure to discuss the risks of lumpectomy with your healthcare provider before you have surgery. Risks may include:
-
Infection
-
Nerve pain
-
Numbness
-
Scar tissue at the surgical site
-
Changes in breast shape. Talk with your healthcare provider before surgery about how your breast shape may change. You may be able to have reconstruction surgery to make your breasts look more similar.
-
Fluid that collects in the breast (seroma)
-
Lymphedema if lymph nodes are removed
When to call your healthcare provider
Talk to your healthcare provider about what problems to watch for. Call right away if you have any of the following:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Increased pain, warmth, drainage, swelling, or redness at the incision
-
Incision opens up or the edges pull apart
-
Cough or shortness of breath
-
Chest pain
-
Any unusual bleeding or bleeding that soaks the dressing
-
Trouble passing urine or changes in how your urine looks or smells
-
Pain, redness, swelling, or warmth in an arm or leg
-
Any other problems your provider told you to watch for and report
Know what problems to watch for and when you need to call your healthcare provider. Make sure you know what number to call anytime you have questions or problems, including after office hours, on weekends, and on holidays.